Bursa Foot Problems
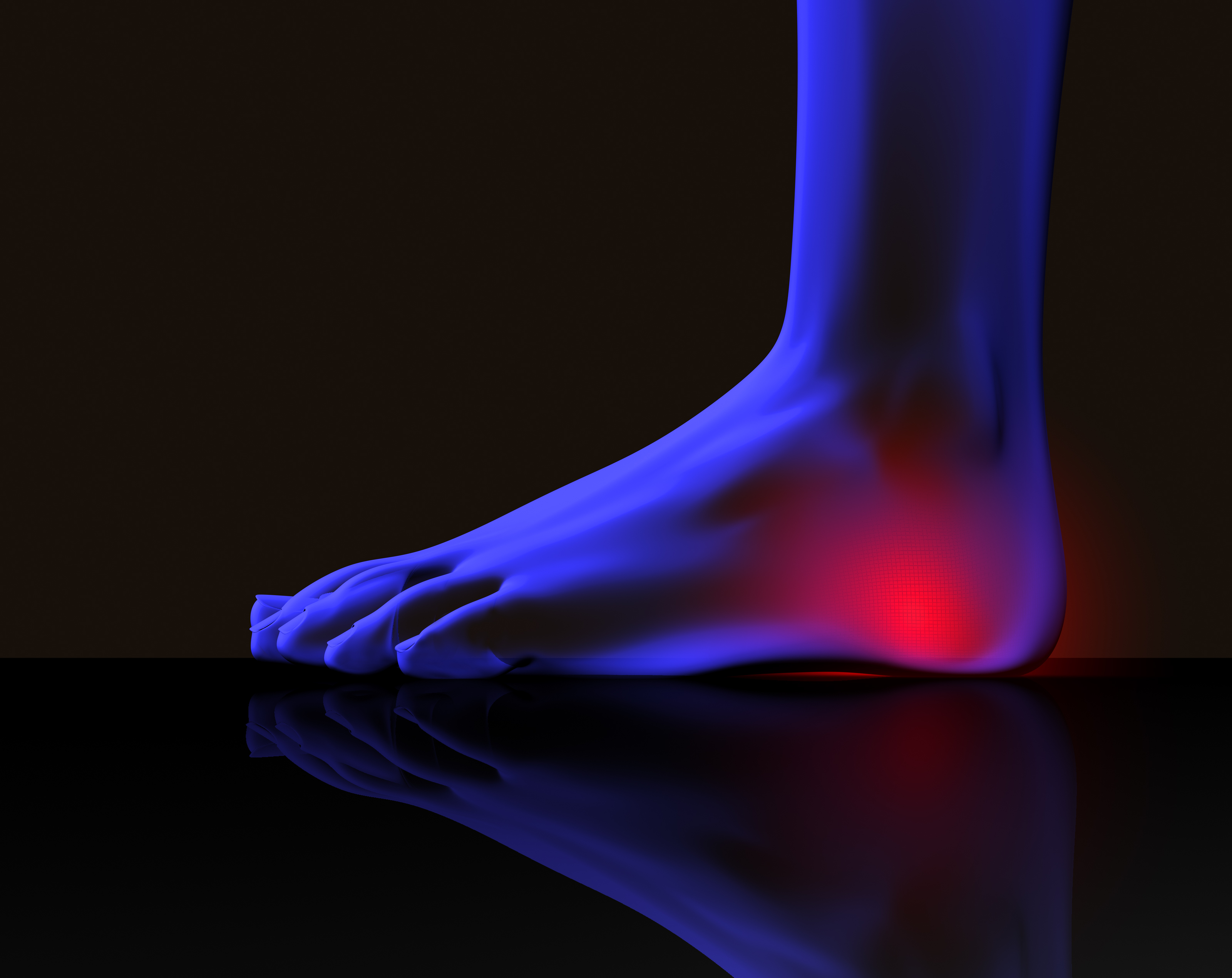
Achilles bursitis is one of those injuries that can really bring down the quality of your life. Anyone, young or old, can suffer from this injury, and if you're active this condition will keep you from doing the things you love to do. It will even start interrupting any of your normal daily tasks and make living life harder than it really needs to be. Fortunately for you, professional athletes have had access to state of the art treatment therapies for years that allow them to heal more quickly and completely than you or I. This is why athletes that have a serious heel bursitis injury can often get back in the game in a matter of weeks while you could suffer for months or even years (in chronic cases).
Causes
Repetitive, vigorous movement, strenuous and unaccustomed activities that put pressure on a joint, or a blow or other injury can bring on bursitis. The cause can vary depending on where the bursitis occurs. In the shoulder, for example, it can be brought on by excessive strain, such as from serving in tennis. Kneeling on a hard floor can cause bursitis of the knee, and similarly, repeatedly resting the elbow on a hard surface (such as a desk) can cause bursitis in that joint. Arthritis, gout, and certain infections can also contribute to the problem. Bursitis, in fact, may signal the onset of arthritis. While getting older isn't a cause of bursitis, older people, especially older athletes, are more likely to develop the condition.
Symptoms
What are the symptoms of heel bursitis? pain, swelling, tenderness, redness, and/or warmth at either the bottom of the heel or top of the heel, depending on the degree of swelling, pain may be a dull ache or substantial enough to cause limping, running, jumping, and walking activities may exacerbate pain, wearing poorly fitting, tight, or high-heeled shoes may exacerbate pain.
Diagnosis
If heel pain has not responded to home treatment, X-rays may be ordered. These images can show deformities of the heel bone and bone spurs that have developed at the attachment of the Achilles. If there is swelling and/or pain that is slightly higher and within the Achilles tendon itself, an MRI may be ordered to determine if the tendon is simply inflamed or if there is a chronic tear on the tendon. Aspiration and lab tests. If a septic bursitis is highly suspected, a doctor may perform an aspiration, removing fluid from the bursa with a needle and syringe. In addition to relieving pressure and making the patient more comfortable, it provides a fluid sample that can be tested for infection.
Non Surgical Treatment
The following exercises are commonly prescribed to patients with retrocalcaneal bursitis. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 2, 3 times daily and only provided they do not cause or increase symptoms. Your physiotherapist can advise when it is appropriate to begin the initial exercises and eventually progress to the intermediate, advanced and other exercises. As a general rule, addition of exercises or progression to more advanced exercises should take place provided there is no increase in symptoms. Move your foot and ankle up and down as far as you can go without pain and provided you feel no more than a mild to moderate stretch. Repeat 10, 20 times provided there is no increase in symptoms. Move your foot and ankle in and out as far as you can go without pain and provided you feel no more than a mild to moderate stretch. Repeat 10, 20 times provided there is no increase in symptoms. Move your foot and ankle in a circle as large as you can go without pain and provided you feel no more than a mild to moderate stretch. Repeat 10, 20 times in both clockwise and anticlockwise directions provided there is no increase in symptoms. Calf Stretch with Towel. Begin this stretch in long sitting with your leg to be stretched in front of you. Your knee and back should be straight and a towel or rigid band placed around your foot as demonstrated. Using your foot, ankle and the towel, bring your toes towards your head as far as you can go without pain and provided you feel no more than a mild to moderate stretch in the back of your calf, Achilles tendon or leg. Hold for 5 seconds and repeat 10 times at a mild to moderate stretch provided the exercise is pain free.
Surgical Treatment
Surgery. Though rare, particularly challenging cases of retrocalcaneal bursitis might warrant a bursectomy, in which the troublesome bursa is removed from the back of the ankle. Surgery can be effective, but operating on this boney area can cause complications, such as trouble with skin healing at the incision site. In addition to removing the bursa, a doctor may use the surgery to treat another condition associated with the retrocalcaneal bursitis. For example, a surgeon may remove a sliver of bone from the back of the heel to alter foot mechanics and reduce future friction. Any bone spurs located where the Achilles attaches to the heel may also be removed. Regardless of the conservative treatment that is provided, it is important to wait until all pain and swelling around the back of the heel is gone before resuming activities. This may take several weeks. Once symptoms are gone, a patient may make a gradual return to his or her activity level before their bursitis symptoms began. Returning to activities that cause friction or stress on the bursa before it is healed will likely cause bursitis symptoms to flare up again.
Hammer Toe Pain
 Overview
Overview
There are two different types of hammertoes. Flexible Hammer Toes. These hammer toes are less serious because they can be diagnosed and treated while still in the developmental stage. They are called flexible hammer toes because they are still moveable at the joint. Rigid Hammer Toes. This variety is more developed and more serious than the flexible condition. Rigid hammer toes can be seen in patients with severe arthritis, for example, or in patients who wait too long to seek professional treatment. The tendons in a rigid hammer toe have become tight, and the joint misaligned and immobile, making surgery the usual course of treatment.
Causes
Though hammer toes are principally hereditary, several other factors can contribute to the deformity. Most prevalent is an imbalance of the muscles and tendons that control the motion of the toe. When the tendon that pulls the toe upward is not as strong as the one that pulls it downward there is a disparity of power. This forces the toe to buckle and gradually become deformed. If the it persists, the toe can become rigid and harder to correct.
 Symptoms
Symptoms
People who have painful hammertoes visit their podiatrist because their affected toe is either rubbing on the end their shoe (signaling a contracted flexor tendon), rubbing on the top of their shoe (signaling a contracted extensor tendon), or rubbing on another toe and causing a painful buildup of thick skin, known as a corn.
Diagnosis
The earlier a hammertoe is diagnosed, the better the prognosis and treatment options. Your doctor will be able to diagnose your hammertoe with a simple examination of the foot and your footwear. He or she may take an x-ray to check the hammertoes severity of the condition. You may also be asked about your symptoms, your normal daily activities, and your medical and family history.
Non Surgical Treatment
Apply a commercial, non-medicated hammer toe pad around the bony prominence of the hammer toe to decrease pressure on the area. Wear a shoe with a deep toe box. If the hammer toe becomes inflamed and painful, apply ice packs several times a day to reduce swelling. Avoid heels more than two inches tall. A loose-fitting pair of shoes can also help protect the foot while reducing pressure on the affected toe, making walking a little easier until a visit to your podiatrist can be arranged. While this treatment will make the hammer toe feel better, it is important to remember that it does not cure the condition. A trip to the podiatrist's office will be necessary to repair the toe to allow for normal foot function. Avoid wearing shoes that are too tight or narrow. Children should have their shoes properly fitted on a regular basis, as their feet can often outgrow their shoes rapidly.
Surgical Treatment
In advanced cases in which the toe has become stiff and permanently bent, the toe can be straightened with surgery. One type of surgery involves removing a small section of the toe bone to allow the toe to lie flat. Surgery for hammertoe usually is classified as a cosmetic procedure. Cosmetic foot surgeries sometimes result in complications such as pain or numbness, so it's better to treat the problem with a shoe that fits properly.
 Prevention
Prevention
Prevention of a hammertoe can be difficult as symptoms do not arise until the problem exists. Wearing shoes that have extra room in the toes may eliminate the problem or slow down the deformity from getting worse. Sometimes surgery is recommended for the condition. If the area is irritated with redness, swelling, and pain some ice and anti-inflammatory medications may be helpful. The best prevention may be to get advice from your podiatrist.
How To Get Rid Of Bunions
Overview
 The original definition of a bunion was a bursa (a fluid-filled sac) on the side of the foot near the base of the big toe. The bursa was caused by a chronic friction of the patient's first metatarsal bone (the bone to which the big toe attaches) and the shoe. Few people go by this definition any longer. Today most people consider a bunion to be the enlarged bone on the side of the foot that typically caused the bursa. Along with this bump, there is usually an associated mis-alignment of the big toe, with it leaning in towards the second toe. In medical jargon, the term for a bunion is "Hallux Abducto Valgus," or "HAV" for short. Though the condition is really slightly different, it may also be known as "Hallux Valgus." Bunions are usually a progressive problem, and can make it difficult to find shoes that fit. The condition is often quite uncomfortable, not only because of the pressure the shoes exert on the bump, but because of the other factors associated with bunions, which we shall discuss shortly. This is usually a progressive problem, and can make it difficult to find shoes that fit. The condition is often quite uncomfortable, not only because of the pressure the shoes exert on the bump, but because of the other factors associated with bunions, which we shall discuss shortly.
The original definition of a bunion was a bursa (a fluid-filled sac) on the side of the foot near the base of the big toe. The bursa was caused by a chronic friction of the patient's first metatarsal bone (the bone to which the big toe attaches) and the shoe. Few people go by this definition any longer. Today most people consider a bunion to be the enlarged bone on the side of the foot that typically caused the bursa. Along with this bump, there is usually an associated mis-alignment of the big toe, with it leaning in towards the second toe. In medical jargon, the term for a bunion is "Hallux Abducto Valgus," or "HAV" for short. Though the condition is really slightly different, it may also be known as "Hallux Valgus." Bunions are usually a progressive problem, and can make it difficult to find shoes that fit. The condition is often quite uncomfortable, not only because of the pressure the shoes exert on the bump, but because of the other factors associated with bunions, which we shall discuss shortly. This is usually a progressive problem, and can make it difficult to find shoes that fit. The condition is often quite uncomfortable, not only because of the pressure the shoes exert on the bump, but because of the other factors associated with bunions, which we shall discuss shortly.
Causes
Improper footwear. Podiatric physicians have long believed that narrow, poor-fitting shoes with a tight toe box tend to compress the end of the foot, leading to abnormal motion of the foot and pressure over the MTP joint. High-heeled shoes tend to add even more pressure to the toes, as the foot slides downward. Over time, continued pressure will squeeze the toes together, encouraging the deformity. Occupational hazards. Individuals whose jobs place undue stress on their feet are among those who complain of bunions. Ballet dancers, in particular, put great demands on their toes, and thus are often subject to bunions, however, they are not alone. Many professionals whose jobs require a great deal of standing or walking (teachers, police officers, doctors and nurses, etc.) and/or who are required to wear a particular type of shoe or boot as part of a uniform, also are at risk. Athletes such as runners or walkers, who utilize the wrong footwear, may also develop bunions.
Symptoms
Bunions may or may not cause symptoms. A frequent symptom is foot pain in the involved area when walking or wearing shoes that is relieved by resting. A bunion causes enlargement of the base of the big toe and is usually associated with positioning of the big toe toward the smaller toes. This leads to intermittent or chronic pain at the base of the big toe. Bunions that cause marked pain are often associated with swelling of the soft tissues, redness, and local tenderness. It is important to note that, in post-pubertal men and post-menopausal women, pain at the base of the big toe can be caused by gout and gouty arthritis that is similar to the pain caused by bunions.
Diagnosis
Before examining your foot, the doctor will ask you about the types of shoes you wear and how often you wear them. He or she also will ask if anyone else in your family has had bunions or if you have had any previous injury to the foot. In most cases, your doctor can diagnose a bunion just by examining your foot. During this exam, you will be asked to move your big toe up and down to see if you can move it as much as you should be able to. The doctor also will look for signs of redness and swelling and ask if the area is painful. Your doctor may want to order X-rays of the foot to check for other causes of pain, to determine whether there is significant arthritis and to see if the bones are aligned properly.
Non Surgical Treatment
Getting rid of a Bunion is almost impossible without surgery. Foot and toe exercises can help. Foam pads can reduce the pressure on the joint. Ice packs and anti-inflammatory medication can help reduce swelling. The progress of a Bunion can be slowed or even halted, especially if it is caused by ill-fitting footwear. Of course the best course of action is to not wear pointy-toed high-heel shoes to begin with. But if you have worn improper footwear and now want to stop the progress of Bunions. 
Surgical Treatment
Complications of bunion surgery are not common, but include infection of soft tissue and/or bone, slow healing of skin or bone, irritation from fixation pins or screws, nerve entrapment, reaction to the foreign material (suture material, pins or screws), excessive swelling, excessive scarring, excessive stiffness (some stiffness is unavoidable), over-correction (hallux varus) and recurrence of the deformity. Rarely, some complications may require a second surgery to correct the problem. While these complications are rare, they should be weighed against the difficulty that you are experiencing to determine whether surgery is an acceptable risk for your condition. This is an important part of the process.
Overpronation Of The Feet
Pes planus is the medical term for flat feet. It comes from Latin, Pes = foot and Planus = plain, level ground. Very few people suffer from this condition, as a true flat foot is very rare. Less than 5% of the population has flat feet. The majority of the population, however, has fallen arches (an estimated 60-70% of the population) known in the medical profession as ?excess pronation? or over-pronation. Over-pronation means the foot and ankle tend to roll inwards and the arch collapses with weight-bearing. This is a quite a destructive position for the foot to function in and may cause a wide variety of foot, leg and lower back conditions.
Causes
Congenital "Flat Feet" - an individual may be born with feet that lack an appropriately supportive arch thereby predisposing the individual to this foot condition. Excessive Weight (Obesity) Too much weight on the foot from either obesity or pregnancy may be a factor. Repetitive Impact walking on flat, hard surfaces continuously places unnatural stress on the foot arch.
Symptoms
In addition to problems overpronation causes in the feet, it can also create issues in the calf muscles and lower legs. The calf muscles, which attach to the heel via the Achilles tendon, can become twisted and irritated as a result of the heel rolling excessively toward the midline of the body. Over time this can lead to inflexibility of the calf muscles and the Achilles tendon, which will likely lead to another common problem in the foot and ankle complex, the inability to dorsiflex. As such, overpronation is intrinsically linked to the inability to dorsiflex.
Diagnosis
If you have flat feet or low arches, chances are you overpronate. Although not always the case, the lower your arches the greater the overpronate. Stand on a hard surface (in front of a mirror if you need to) and look at your feet, flat feet or low arches are easy to spot. If your feet look flatter than a pancake, have a look at your ankles and see if they seem collapsed or straight. If they are, you're overpronating.

Non Surgical Treatment
Side Step with Opposite Reach. This exercise is designed to load the "bungee cord system" of the gluteal muscle and its opposite, latissimus dorsi muscle to keep the foot from overpronating. Because the opposite arm swings across the front leg when walking, this exercise creates tension in the muscles all the way from the front foot, across the back of the hips and back, to the fingers of the opposite hand. Movement Directions. Stand with left foot on top of the dome of the BT. (Note: For added balance, the right foot can tap on the ground, if needed). Reach right leg out to the side of the BT, and tap the ground while squatting down on the left side and reaching right arm across the left knee. Push down with left big toe while squatting. This activates the arch of the left foot and strengthens all the stabilizing muscles on the left side of the lower body. Return to starting position. Perform 8 to 10 repetitions on each leg.
Surgical Treatment
Depending on the severity of your condition, your surgeon may recommend one or more treatment options. Ultimately, however, it's YOUR decision as to which makes the most sense to you. There are many resources available online and elsewhere for you to research the various options and make an informed decision.
Physical Rehabilitation And Calcaneal Apophysitis
Sever?s disease or Sever?s lesion refers to an injury to the bone growth plate at the back of the heel bone (calcaneous) in young people, particularly those who are physically active. It usually develops in puberty and is slightly more common in boys than girls.
Causes
There is no specific known cause of Sever?s disease. However, there are several common factors associated with the condition including. Tight calf muscles. Pronated foot type (rolled in towards the ankle). Children who are heavier. Puberty/growth spurts. External factors, e.g. hard surfaces or poor footwear. Increase in physical activity levels.
Symptoms
Some of the most common signs and symptoms associated with Sever?s disease include. Heel pain or tenderness in one or both heels, usually at the back of the heel. Pain or discomfort upon waking, or when the heel is squeezed. Heel pain that is worse during or following activity. Limping. Heel swelling or redness. Tight calf muscles. Decreased ankle range of motion.
Diagnosis
A doctor can usually tell that a child has Sever's disease based on the symptoms reported. To confirm the diagnosis, the doctor will probably examine the heels and ask about the child's activity level and participation in sports. The doctor might also use the squeeze test, squeezing the back part of the heel from both sides at the same time to see if doing so causes pain. The doctor might also ask the child to stand on tiptoes to see if that position causes pain. Although imaging tests such as X-rays generally are not that helpful in diagnosing Sever's disease, some doctors order them to rule out other problems, such as fractures. Sever's disease cannot be seen on an X-ray.
Non Surgical Treatment
Depending on the Podiatrist's diagnosis and the severity of the pain, there are several treatment options available. Rest/ reduced activity: your child should reduce or stop any activity that causes pain, such as sports and running. This can be a difficult option, as children are normally quite willful in pursuit of their favorite pastimes! Over the counter anti-inflammatory drugs, such as ibuprofen (found in Nurofen), to help reduce pain and inflammation. Try to make sure your child does the recommended stretching exercises before sport/play. This will should help reduce the stress on the fascia tendon and relieve heel pain. The use of Orthotic insoles. Footactive Kids orthotics are made for children. They will help properly support the foot, help prevent over-pronation or improper gait restoring your child's foot the the correct biomechanical position. If you are in any doubt or your child's foot pain persists then please arrange an appointment with a Podiatrist or Physiotherapist. Please click here for more information on the use of orthotics for children.
Posterior Tibial Tendon Insufficiency Treatment
Overview
PTTD is a condition of degeneration and dysfunction in the tendon complex that helps control the medial arch of your foot. Essentially what happens is the complex is unable to do its job of supporting the arch and supinating the foot, so a progressive flat foot develops (usually called adult acquired flat foot). Initially pain and often swelling develops on the inside of the ankle and it will continue to get progressively worse. There are a number of stages of PTTD (3 Stages) and it needs to be aggressively treated early on otherwise a surgical reconstruction of the arch will invariably be required. PTTD can develop into a very disabling condition if it is not dealt with properly and promptly. As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. Arthritis often develops in the foot and In more severe cases, arthritis may also develop in the ankle. 
Causes
Posterior tibial tendon dysfunction is the most common cause of acquired adult flatfoot. Sometimes this can be a result of specific trauma, but usually the tendon becomes injured from wear and tear over time. This is more prevalent in individuals with an inherited flat foot but excessive weight, age, and level of activity are also contributing factors.
Symptoms
In many cases, adult flatfoot causes no pain or problems. In others, pain may be severe. Many people experience aching pain in the heel and arch and swelling along the inner side of the foot.
Diagnosis
It is of great importance to have a full evaluation, by a foot and ankle specialist with expertise in addressing complex flatfoot deformities. No two flat feet are alike; therefore, "Universal" treatment plans do not exist for the Adult Flatfoot. It is important to have a custom treatment plan that is tailored to your specific foot. That starts by first understanding all the intricacies of your foot, through an extensive evaluation. X-rays of the foot and ankle are standard, and MRI may be used to better assess the quality of the PT Tendon.
Non surgical Treatment
Non-surgical treatment consists of custom orthoses and or special bracing devices along with supportive measures aimed at reducing the symptoms. While non-surgical treatment helps the majority of patients with PTTD, progressive cases may require surgical treatment including soft tissue tendon transfers, osteotomies and lastly fusion. 
Surgical Treatment
For more chronic flatfoot pain, surgical intervention may be the best option. Barring other serious medical ailments, surgery is a good alternative for patients with a serious problem. There are two surgical options depending on a person?s physical condition, age and lifestyle. The first type of surgery involves repair of the PTT by transferring of a nearby tendon to help re-establish an arch and straighten out the foot. After this surgery, patients wear a non-weight bearing support boot for four to six weeks. The other surgery involves fusing of two or three bones in the hind foot below the ankle. While providing significant pain relief, this option does take away some hind foot side-to-side motion. Following surgery, patients are in a cast for three months. Surgery is an effective treatment to address adult-acquired flatfoot, but it can sometimes be avoided if foot issues are resolved early. That is why it is so important to seek help right away if you are feeling ankle pain. But perhaps the best way to keep from becoming flatfooted is to avoid the risk factors altogether. This means keeping your blood pressure, weight and diabetes in check.
Sharp Pain In Right Foot Arch
Painful progressive flatfoot, otherwise known as Tibialis Posterior Tendinitis, is caused by inflammation of the tendon of the tibialis posterior. The tendon then becomes inflamed, stretched or suffers a partial or total tear. If left untreated, this condition may lead to severe disability and chronic pain. Some people are predisposed to this condition if they have flatfeet or an abnormal attachment of the tendon to the bones in the midfoot. Nonsteroidal anti-inflammatory medications, ice, physical therapy, supportive taping and bracing, or orthotic devices are the common ways of treating painful progressive flatfoot. Contact your physician before taking any medication. In some cases, a surgical operation may need to be performed to repair the torn or damaged tendon and restore normal function. To prevent reinjury, orthotic devices may be recommended. In severe cases, surgery on the midfoot bones may be necessary to treat the associated flatfoot condition.

Causes
Plantar fasciitis, another sports injury detailed on this website, is regularly the cause of foot arch pain or strain. This can arise due to faulty biomechanics in your feet, which alone can also provoke foot arch pains. The most prominent biomechanical difficulties are flat feet and high arches. With flat feet (or overpronation) the arches appear to be almost flattened, causing unevenness by forcing the feet roll inwards in order to maintain balance and support the body's weight. This places inordinate pressure on the plantar fascia and arches. If by contrast you have high arches (instep), the ankle can roll outwards, again causing undue strain on the arches. Too much of this strain can lead to stretching of the plantar fascia and pain in the arches. Other causes include overstretching or otherwise pressuring the arches, for example by exercising with fatigued leg muscles which leave the feet with excessive work to do. You are also particularly at risk if in your 40s or 50s and commencing an intense program of training after a long period of inactivity.
Symptoms
Repetitive exertive activity arch pain is usually sharp, and localized to a specific area, rather than the entire arch. Usually the pain occurs in the area just in front of the heel. It is present when first standing on the foot in the morning, but may decrease once you start walking around, but will, gradually becomes worse with continued walking or running. Swelling may be present. The pain subsides with rest, but stretching the arch while resting may cause the pain to return. Injury pain is constantly present, but worse when standing on the foot. This pain is localized to a specific area, but may radiate out from this area to the entire foot. The pain is sharp, and usually accompanied by swelling and occasionally "black and blue" discolorations. The pain due to the natural aging process is usually dull and aching, or stiff, and can be felt throughout the entire arch area, rather then in just one spot. This pain is present whenever weight bearing, and usually becomes worse with continued walking. The pain gradually subsides when resting, and usually does not return with stretching. Biomechanical defect pain is usually localized to a section of the arch, such as the inner, middle, outer, front, or back of the arch. This pain may be sharp or dull, but is always worse with continued walking.
Diagnosis
The adult acquired flatfoot, secondary to posterior tibial tendon dysfunction, is diagnosed in a number of ways with no single test proven to be totally reliable. The most accurate diagnosis is made by a skilled clinician utilizing observation and hands on evaluation of the foot and ankle. Observation of the foot in a walking examination is most reliable. The affected foot appears more pronated and deformed compared to the unaffected foot. Muscle testing will show a strength deficit. An easy test to perform in the office is the single foot raise.
Non Surgical Treatment
How the pain in the bottom of your foot is treated will depend heavily on the cause of the pain. Diagnosing the pain while it?s in the early stages is important when determining the best treatment options. If the pain is mild to moderate, simple improvements in footwear can help reduce the symptoms. Most patients must use the RICE method for effective treatment. RICE stands for Rest, Ice, Compression, and Elevation. This is a popular treatment used by athletes. It involves resting the foot, icing it for fifteen to twenty minute intervals, compressing the foot with a bandage, and elevating it at least twelve inches above the heart. Ant-inflammatory and pain medications are also sometimes used to treat bottom-of-foot pain. For more serious cases, steroid injections or foot surgery may help reduce pain and swelling and correct the underlying condition (if there is one.) If you suffer from a severe case of plantar fasciitis and non-surgical methods fail, your doctor may recommend cortisone injections to relieve the pain. If cortisone injections fail, your doctor may recommend a surgical procedure that involves cutting and releasing the plantar fascia.

Surgical Treatment
Cavus foot is caused in part by an over-pull of one of the lateral ankle muscles. A release of this tendon can be performed on the outside of the ankle. Additionally, a transfer of this tendon can be performed to help in correcting deformity of the ankle joint. Often patients will have a tightness of their gastrocnemius muscle, one of the main muscles in the calf. This can increase the deformity or prevent a correction from working. It is addressed with a lengthening of a part of the calf muscle or Achilles tendon. This is often performed through one or more small cuts in the back of the leg or ankle. Finally, the plantar fascia may be tight. The plantar fascia is a cord-like structure that runs from the heel to the front part of the foot. Partial or complete plantar fascia release may be done.
Prevention
Foot and ankle injuries are common in sports, especially running, tennis and soccer. But sports enthusiasts can decrease the risk of injury by taking some precautions. Lightly stretch or better yet, do a slow jog for two to three minutes to warm up the muscles. Don't force the stretch with a "bouncing motion." The amount of time spent on the activity should be increased gradually over a period of weeks to build both muscle strength and mobility. Cross training by participating in different activities can help build the muscles. People whose feet pronate or who have low arches should choose shoes that provide support in both the front of the shoe and under the arch. The heel and heel counter (back of the shoe) should be very stable. Those with a stiffer foot or high arches should choose shoes with more cushion and a softer platform. Use sport-specific shoes. Cross training shoes are an overall good choice; however, it is best to use shoes designed for the sport.
Stretching Exercises
Easy Beginner Version. Start with your bare foot on a flat surface, toes spread out. Place a penny under the ball of your foot and the end of a pen under the middle of your arch (sticking out from the inside of your foot). Activate your arch by flexing your arch muscle. You should feel the muscles on the ball of your foot pushing down on the penny, but your arch shouldn't be pushing down on the pen. These tools help you (1) avoid rolling your foot and (2) avoid pressing down with your toes (as an extra tip, you can slide a business card under your toes before doing the exercise-when you activate your arch, you should be able to slide the business card out easily with your fingers). Do your best to keep your toes relaxed. Advanced Version. Once you're ready to move on, you can try this advanced version. It builds on the above exercise to incorporate full body twisting and balance, helping you to maintain proper arches while you move. Using the same ideas from above, stand on a flat surface in your bare feet with a penny under the ball of your foot and the end of a pen under your arch. This time, stand with your back a few inches away form a wall or a door. Lift your other leg (the one without the penny or pen) and stand on one foot. Use the wall for balance, if necessary. Lift one arm and stretch it across your body until you touch the wall or door on the opposite side, maintaining a straight back. Keep your foot straight and your arch on the penny but above the pen. Your arch will want to follow the movement and roll off, but you will need to activate it to stay stable during the movement. Lift your other arm and stretch it across the opposite side of your body, still keeping your arch in place.